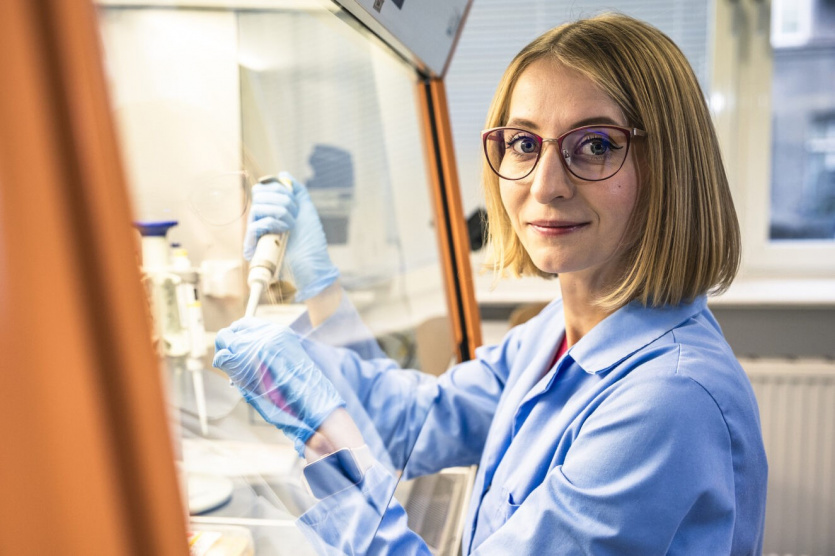
Katarzyna Dziubek in the laboratory; photo: Alan Stocki/UG.
Cancer is a complex and devious disease, constantly evolving and trying to trick our immune system. It comes in many varieties, characterised by numerous genetic mutations. A doctoral student at the Intercollegiate Faculty of Biotechnology UG and MUG and a researcher at the International Centre for Anticancer Vaccine Research at the University of Gdańsk, mgr Katarzyna Dziubek, is investigating the mechanism potentially responsible for the ineffectiveness of immunotherapy in some osteosarcoma patients and many other kinds of cancer. In the future, her research may help develop an effective therapy and thus contribute to saving the lives of young patients and animals most commonly affected by this cancer. We encourage you to read the next talk in the series 'Young UG Scientists'.
Elżbieta Michalak-Witkowska: - You are a pharmacist by training, but you work scientifically in the areas of biotechnology, molecular biology, and cell biology. Currently, at the UG's International Centre for Cancer Vaccine Science, you are researching osteosarcoma - a rare type of cancer that primarily affects children and young adults. How did it come about that you are carrying out this important research at UG?
Katarzyna Dziubek: - My studies started in Łódź, and my major then was Pharmacy. In my third year, I joined the scientific circle in the Department of Pharmaceutical Chemistry, and there, my future thesis supervisor encouraged me to travel and contact other research centres. This is how cooperation with Charles University in Prague began, where I carried out part of the research for my thesis. Then, I went for a year-long internship to the United States, where I conducted research on the cell cycle. Upon my return, there was an advertisement for a PhD student position at UG, and as the project was interesting, I did not think long about sending in my application.
- Your PhD title is 'Analysis of the Signalling Mechanism and Function of the PD1 Receptor in Osteosarcoma'. You are pursuing it at ICCVS in collaboration with the University of Edinburgh, where you started your research. What exactly are you investigating?
- I am investigating the role of the PD1 receptor found on osteosarcoma cells and trying to establish whether it is the reason why immunotherapy has been unsuccessful in this cancer. Importantly, my research may not only be applicable to this type of cancer but also to many others that produce the PD1 receptor. To explain this better, a brief introduction will be necessary. In recent years, PD1/PDL1 immunotherapy has proved to be a revolution in cancer treatment and has already helped many patients. It targets the PD1 receptor - a protein on the surface of immune cells, mainly cytotoxic T lymphocytes, which are responsible for killing cells recognised as foreign, including cancer cells. The PD1 receptor, when activated by its ligand PDL1, regulates their function by acting as a brake on immune cells. This is exploited by the well-known mechanism of action of immunotherapy. Only with time was it discovered that the PD1 receptor is also found on cancer cells. It may, therefore, affect the effectiveness of PD1/PDL1 immunotherapy, but we still do not fully understand how it works.
- So, the PD1 receptor acts as a gatekeeper for our immune system?
- It is called the programmed cell death (PD1) receptor or immune checkpoint. PD1 function is crucial to maintain control of the immune system. Insufficient activity of the receptor leads to the over-activation of T cells, resulting in the destruction of our own tissues through an autoimmune response. However, in cancer, we do not want the PD1 receptor to over-inhibit immune cells capable of eliminating the tumour. Therefore, we use PD1/PDL1 immune therapy, which blocks either the PD1 receptor or its ligand, helping immune cells regain their ability to kill cancer cells. Based on this principle, we observe a therapeutic effect.
- Why did you choose osteosarcoma for your research?
- Because it is a rare disease and no significant progress has occurred in its treatment since the 1970s. In addition, my collaboration with the Roslin Research Institute, during which I studied tumour mechanisms in dogs (I mean animals that came to the clinic with already developed tumours), showed that osteosarcoma follows a similar course in animals as in humans and that it is a very similar disease in terms of pathomorphology. Dogs are exposed to similar environmental risk factors; moreover, the condition is 27 times more common in them than in us. Developing a therapy for them will help both them and us, so in part, this is comparative research.
- It seems to be challenging to find a suitable, effective therapy for cancer. What might this be due to?
- It is a very multi-component and complex disease. In addition, cancers are constantly evolving; they are sneaky and look for ways to trick our immune system. And they have specialised well in this. Tumours have learned to activate the PD1 receptor on T cells by producing a ligand for PD1, a molecule that binds to the receptor and activates it. The reaction between the ligand produced by the tumour and the PD1 receptor weakens the immune cells. And they are then unable to recognise the tumour. They do not attack it. In addition, as I mentioned, quite surprisingly, recent studies have shown that the PD1 receptor is present not only on immune cells but also on cancer cells.
- Could the presence of the PD1 receptor on tumour cells be a reason for the ineffectiveness of immunotherapy in some osteosarcoma patients?
- This is the subject of my research. At this point, we have contradictory reports from researchers. Depending on the type of cancer, some have observed that the PD1 receptor present in its cells accelerates the growth of tumour cells, while others have observed that it inhibits it. My role is to resolve this issue. My main focus in my research is to explain why immunotherapy may not have worked in that case. To do this, I am describing the receptor's action in more detail.
- And if your assumptions are confirmed?
- Then it may turn out that immunotherapy is not safe for everyone - or that we will have to make more effort to modify the therapy only to target PD1 on immune cells. However, to be sure whether immunotherapy - which modifies the receptor both in the tumour and immune cells - can harm or help in a given patient, we need to clarify the mechanism of action of PD1 in tumours. I am therefore investigating the function of the PD1 protein and whether this is dependent on the use of therapy. If it turns out that the presence of PD1 on tumour cells negatively affects the response to immunotherapy, we can introduce an additional mechanism to block this function.
- What stage of research are you at?
- I am currently conducting in vitro studies on a human osteosarcoma cell model and will soon move on to the canine bone tumour part. A large part of the research has been and will continue to be done in our laboratory, using the modern LC-MS/MS (liquid chromatography-tandem mass spectrometry) technique, which allows a broad insight into the regulation of the cell's proteins and tracking of key cellular processes. As a next step, I will work on an in vivo model at the University of Edinburgh, where I will analyse cancer cells' virulence. All this, of course, is in the context of the PD1 receptor. Animal studies, already diseased animals, if they occur, will take place further in the future. We want to help dogs that also have bone cancer and are suffering greatly. I have a lengthy research procedure ahead of me. It will undoubtedly be several years before we can apply the therapy to the animals.
- Finally, I would like to ask what you wish for regarding your research.
- I am at the stage of completing my doctoral thesis, so I will soon be sending out my first research results for publication. I hope that my work will see the light of day in the coming months and that I will be able to develop the research in such a way as to create an effective therapy for osteosarcoma with its help. In addition, my research on the PD1 receptor is very likely to find application in other types of cancer – and this is what I wish for.
- In that case, good luck! Thank you for the interview.